Ear eczema

Introduction
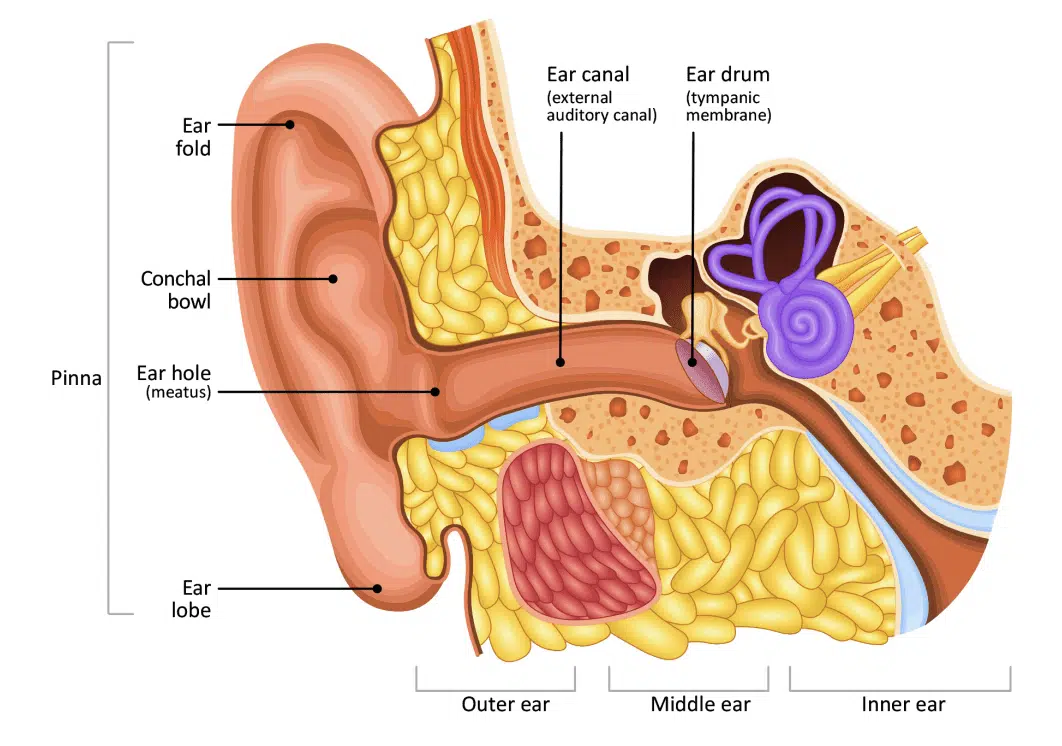
Ear eczema can be an extremely irritating and, at times, painful condition. It can range from slight dryness of the pinna (the visible, projecting part of the ear) to extensive skin loss and soreness, as well as infection of the external and internal parts of the ear. Eczema can affect the entire ear including the earlobes, conchal bowl (the area outside the ear hole), the ear opening (meatus), ear canal (also known as the external auditory canal – the part of the ear that leads to the ear drum) and the ear drum itself (also known as the tympanic membrane). The ear folds, backs of the ears and the area where the ears meet the face are also common areas for eczema.
There are a number of causes of ear eczema and it is always best to consult your doctor if you think you may have it, in order to get effective treatment and prevent flare-ups. Several different types of eczema may affect the ear.
Atopic eczema
The ears and skin behind the ears are frequently affected in people with atopic eczema. As with other areas of the body, the eczematous skin here is dry, itchy and red or darker than a person’s usual skin colour, depending on skin tone. It can easily become infected, especially if the skin is scratched and breaks. A common site of ear eczema in people with atopic eczema is the junction between the earlobe and the face. Eczema in this area can cause painful cracks (fissures) in the skin, which can then easily become infected. Sometimes eczema can affect the whole of the pinna and track down the ear canal.
Seborrhoeic dermatitis
Seborrhoeic dermatitis is a form of eczema triggered by an over-reaction of the skin’s immune system to an overgrowth of a harmless yeast called malassezia that lives on the skin. People who have this type of eczema often have dandruff on the scalp and itchy, flaky skin with a yellowish, greasy scale in typical seborrhoeic dermatitis areas, which include the face (along the smile lines and eyebrows), centre of the chest and sometimes the eyelids and ears.
Around the ears, seborrhoeic dermatitis often takes the form of inflammation of the ear canal and along the hairline behind the ear (the post-auricular area), which can lead to painful fissures or cracks. It can sometimes be confused with psoriasis.
Treatment usually aims to reduce the overgrowth of yeast on the skin. This may include anti-fungal shampoos to wash the skin, and creams that may or may not contain mild topical steroids, such as Daktacort cream, to help reduce inflammation. Topical calcineurin inhibitors (Protopic ointment or Elidel cream) are sometimes used for this form of eczema, although they are not licensed for it.
Asteatotic eczema
This type of eczema affects older people. The exposed ear is vulnerable to changes in weather and temperature, which lead to dry, scaly and itchy skin causing asteatotic eczema. Aggravating factors include over-washing, cold or windy weather, central heating, low humidity indoors and air-conditioning.
Contact dermatitis
The external ear is commonly affected by both irritant and allergic contact dermatitis.
Irritant contact dermatitis comes about when the skin’s surface is irritated by a substance that causes the skin to become dry, itchy and red or darker than a person’s usual skin colour, depending on skin tone. Examples of substances that can cause irritant contact dermatitis around and inside the ears are shampoo, hair gel, hair spray, perm solution, hair colourant and perfume.
Allergic contact dermatitis develops as a result of your body reacting to a particular substance to which you are allergic. Everyday items that can cause allergic contact dermatitis around and inside the ears include the following:
- Products used for the hair and scalp (for example, shampoo, conditioner, gel, hairspray, hair colourant, perm solution, hairpins and grips, hairnets and bathing caps). You might wish to try wearing ear plugs when showering and washing your hair, as these stop products collecting in the ear canal.
- Earrings and studs, especially those containing nickel.
- Plastic, rubber or metal ear appliances (for example, hearing aids and moulds, spectacles, head- and earphones, earbuds and earplugs).
- Objects used to clean or scratch the ear.
- Cosmetics and toiletries (for example, make-up, perfume and soap).
- Topical medications (for example, ointments, creams and gels).
- Allergens transferred to the ears via the fingers (for example, nail varnish and plant resin from poison ivy or oak).
Otitis externa
Also known as ‘swimmer’s ear’, this is an inflammatory condition of the ear canal. It can be caused by a primary skin problem, such as eczema, or by a bacterial or fungal infection. Having ear eczema increases your risk of getting otitis externa too. Other risk factors include swimming, sweating, high humidity and local trauma to the ear canal (for example, by using cotton buds or scratching the inside of the ear).
Symptoms include earache, skin becoming red or darker than your usual skin colour, depending on skin tone, swelling, itching and discharge from inside the ear. In severe cases, it can reduce people’s hearing due to swelling of the ear canal.
In suspected cases, dermatologists may seek help from the ear, nose and throat (ENT) medical team. To avoid getting otitis externa:
- Keep the ear clean.
- Avoid trauma, irritants and allergens.
- Keep the outside of the ear dry – particularly after bathing and swimming.
- Make sure any underlying contributing skin condition is well-controlled.
Ear piercing
Ear piercing does not cause ear eczema, but problems can occur later on as a consequence of wearing earrings or studs. Nickel allergy is very common and the chance of this developing is greatly increased if you have your ears pierced and if anything made even partly from nickel is worn in or on the ear.
If you definitely have a nickel allergy, wear only ‘hypo-allergenic’ jewellery or jewellery made from 18- carat gold, pure sterling silver, platinum or good-quality stainless steel. Foreign silver, rolled gold, white gold and gold plating should be avoided.
Pierced ears can become infected, particularly just after piercing. Make sure you go to a reputable ear-piercing technician to get your ears pierced, and wash the piercings frequently afterwards with the saline solution you were given by the ear-piercing technician.
Treatment of ear eczema
Treatment of ear eczema will depend on the cause and type of eczema, which will need to be diagnosed by your GP.
For atopic, seborrhoeic or asteatotic eczema, apply a medical emollient frequently to the affected areas. You may be prescribed a topical steroid for sore areas behind the ears, and in their folds. If you have seborrhoeic dermatitis, a topical steroid combined with an antifungal may be prescribed.
Topical calcineurin inhibitors, the brand names of which are Protopic and Elidel, are sometimes prescribed for ear eczema.
Apply your topical treatments by using a cotton bud to gently paint your cream or ointment on the affected area. Do not push the cotton bud into your ear.
If you have eczema inside the ear canal, you will need steroid drops, which will be prescribed by your GP or other healthcare professional.
If allergic contact dermatitis is suspected, you may be referred to a dermatology department to help find out what you are allergic to so that you can avoid it in the future. The dermatologist will usually recommend patch testing.
The usual treatment for otitis externa is antibiotic ear drops, which may also contain a steroid to reduce inflammation, itch and swelling. Sometimes a swab is taken to identify the most appropriate antibiotics – particularly if the condition does not improve. The ENT clinic may also clean the ear using gentle suction or irrigation (called ‘aural toilet’).
Cleaning of the ears and self-care
You can very gently wash the inside of your outer ear with water or preferably an emollient wash. You can also apply a damp cotton bud very gently to the bowl area of your ear but do not insert it into the ear canal. Never try to wash further into the ears – you can damage the skin of the ear canal by doing this.
After washing, dry your ears thoroughly. Using a warm (not hot) hairdryer is a good way to ensure your ears are dry. Avoid scratching the inside of your ears, especially with matches or hair grips – not only can these damage your ear canal skin or drum, but they may cause an allergic reaction after continuous use.
The use of ear candles is not advised as there is no evidence to suggest that they work, and they can damage the ears.
If you go swimming, use ear plugs. You can get custom-made ear moulds to fit your ears – they are like the moulds used for hearing aids. Ear moulds can be made and fitted at hearing aid centres. Larger chemists such as Boots provide this service, as do private audiologists.
Olive oil is sometimes recommended for moisturising around the ear pinna and loosening wax. However, medical research evidence shows that olive oil damages the skin barrier. Instead, we recommend applying an emollient to treat dry skin around the ears and in the entrance to the ear canals, and use refined petroleum oil (unfragranced baby oil) or sunflower oil to soften ear wax (but consult first with a healthcare professional). Water is not recommended, nor are wax softener products bought from chemists, as they may encourage the build-up of debris and cause more inflammation and irritation.
Infected ear eczema
Skin affected by eczema and dermatitis can become infected, usually by bacteria, especially if the skin surface is broken due to dryness and scratching. This is similar to eczema infections on other areas of the skin.
Ear eczema that becomes infected can encourage a build-up of wax, skin scales and hair in the ear canal, which can lead to blockage and cause temporary deafness. Infected eczema and ear infections can also come about when the ears are wet for long periods of time. For instance, if you swim a lot and leave your ears damp after swimming or washing your hair, your chances of an ear infection increase. Pressure from hearing aids and earpieces can also encourage ear infection, so try to ensure they are a comfortable fit.
Symptoms of infection inside the ear include earache, itching, pain, the skin becoming red or darker than your usual skin colour, depending on skin tone, weeping, swelling and an unpleasant smell or dirty-coloured discharge (often yellow or green) from inside the ear. If you have any of these signs, make an appointment to see your GP. Please note: ear discharge that is clear is normal if you have ear eczema, especially when eczema is active (weepy eczema).
You may be prescribed a ‘combination’ preparation containing a mixture of antibiotic and topical steroid for bacterial infections, or an antifungal and topical steroid for fungal infections. You should complete the course of treatment.
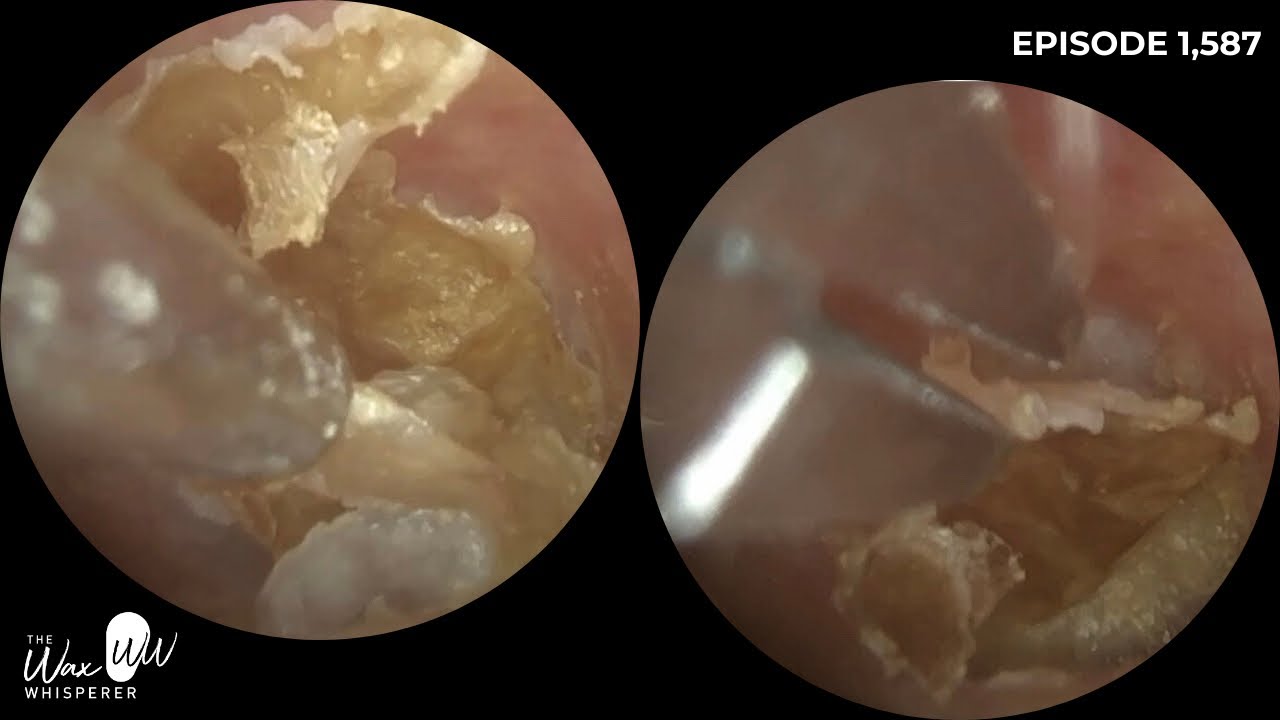
Aural toilet by healthcare professionals
A build-up of wax and flaky skin from patches of eczema can produce a lot of ‘debris’ in the ear canal. This can easily get infected, especially when water is present. So prevention of ear infection is key.
Manual cleaning of the ear by a healthcare professional is called ‘aural toilet’ and is often recommended to remove the debris and scale that can build up in the ear canal. It is done under a microscope, either using a pick or hook (Jobson Horne probe), or microsuction, an electric suction system.
Microsuction is also recommended if ear wax is truly impacted, and is considered safer and definitely better than flushing the ears with water, especially for people with ear eczema. Although many GP practices offer ear syringing and/or ear irrigation (an electronic machine for washing the ears) to remove ear wax, water-based methods are not recommended for people with ear eczema, unless it is very mild. Sometimes regular aural toilet is recommended (once or twice a year) to prevent wax and eczema debris build-up.
Aural toilet can be performed by aural care nurses/technicians, or sometimes by specially trained practice nurses. Ask your GP for a referral to the aural care service (provision may vary around the UK). Alternatively, this service may be provided privately by audiologists – your GP practice may be able to make a recommendation.
In summary
Ear eczema can be an extremely irritating condition and since it is difficult to look into the ears without specialist equipment, it is often hard to know what is going on, particularly in the case of young children.
If the ears become uncomfortable, don’t ignore it – it is always best to see your GP/healthcare professional, who can use a special torch to look inside. Often this will reveal the cause of ear discomfort and the problem can then be resolved, using one of the many treatments available for ear eczema and ear infections.





![Ingrown Nail Tools [ Relaxing Cleaning Nail ] #usa #video #viralvideo](https://usafactsnews.com/wp-content/uploads/2025/02/ppp93-348x215.jpg)


.jpg)
.jpg)
.jpg)
.jpg)
.jpg)







:max_bytes(150000):strip_icc():format(webp)/GettyImages-1214497552-88bad55d76de40b58cd310dadb077f39.jpg)