More information about nail surgery for chronically ingrowing toenails.
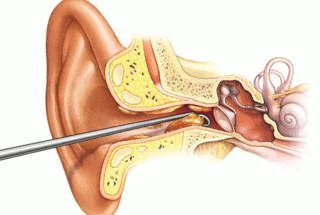
Nail surgery is a procedure to remove either the entire nail plate (total nail avulsion), or slivers from either side of the nail (partial nail avulsion/s), under local anaesthetic.
This can be undertaken by a podiatrist, suitably-trained GP or an orthopaedic surgeon.
You may need to undergo surgery when you develop one of the following conditions:
-
Ingrowing toenail (onychocryptosis)
-
Thickened toenail (onychogryphosis)
-
Severe curvature of the nail (involution)
-
Trauma to the nail (caused by e.g. fungal infection, onychomycosis)
NHS or Private? You can have the procedure under the NHS, or performed privately. The wait time to be seen on the NHS is around 18 weeks for an initial assessment, and the procedure is typically performed 4-6 weeks after that. Privately, such as with Oxfordshire Chiropody, you can be assessed within a week of your enquiry, and the procedure performed a few days later. I am currently making plans for a Straight to Surgery service, to minimise faff without compromising on quality and standards of care.
What happens?
Nail surgery is performed under local anaesthetic; where only the affected toe is injected with anaesthetic and numbed. This is the horrible bit and you will feel a sting. However, you are awake throughout the surgery and you are still be able to feel your toe being moved but you will not feel any pain. The operation takes about 10 minutes however expect the appointment to last 60 minutes. The anaesthetic wears off within a couple of hours.
Most patients tell me they feel no discomfort after the anaesthetic has worn off, but you are free to take paracetamol (as long as this is not contraindicated for you) to keep any discomfort at bay.
There are two types of nail surgery:
-
Partial nail avulsion – removal of one or both sides of the nail affected
-
Total nail avulsion – complete removal of the affected nail
Will the nail grow back?
Once the whole of the nail or part of the nail is removed, phenol is applied to the nail bed and should ensure that the nail does not re-grow. Phenol kills off the ‘nail-making’ cells in the nail matrix. There is a very small chance the nail will regrow, despite using phenol, but this is rare (5%).
Before Nail Surgery Ideally, any soft tissue infection should have been dealt with (antibiotics) prior to surgery. This is just because an infection will change the pH of the skin and can stop the anaesthetic from working effectively. This is one reason why I always ask to see you for an initial appointment before proceeding to nail surgery.
On the day You should eat as normal. Please arrange transport home, as you are not insured to drive whilst your toe is numb following nail surgery. A parent or guardian must accompany patients under sixteen years of age. Plan to rest with your feet up for the rest of the day. Bring a pair of open-toed sandals or a slipper with the toe area cut out.
After Nail Surgery
On returning home, rest with your foot up until the following day.
Do not remove the dressing; keep it clean and dry until your next visit (usually within 2 days of surgery). If there is oozing through the dressing, add an additional dressing on top (which will be provided on the day of surgery).
Take Paracetamol-based painkillers to ease any pain or throbbing.
Avoid walking long distances, kicking, swimming, running or jumping in the early stages of healing (first 2 weeks).
It normally takes around 4 – 6 weeks for the toe to heal, but if you have any concerns after surgery these can be discussed at your dressing appointments.

Considerations before Nail Surgery You will be required to redress your own toe/s every other day for a minimum of 2 weeks. Can you bend down to achieve this? If not, this does not preclude you from surgery but other arrangements will need to be made, such as seeing a Practice Nurse or asking for help from a family member. If you require routine footcare anyway, and have not suffered any nasty infections second to problems with your ingrowing toenails, long-term conservative care may be a better option for you. This is a regular visit to a podiatrist, typically every 6-8 weeks to keep your feet in tip-top shape. The problematic nails can be gently and painlessly ‘resected’ at each appointment. This involves removing a sliver of nail on the oblique, so that as the nail grows, it does so away from the flesh of the toe. If you would like to know more about Nail Surgery, please get in touch