How to Get Rid of Blackheads on the Nose, According to Dermatologists
:max_bytes(150000):strip_icc():format(webp)/VWH-GettyImages-1472202507-0433a042a0754b67adeb19af2b2f21c5.jpg)
- Blackheads are one of the most common forms of blemishes associated with acne that can occur on the face, nose, neck, back, and chest.
- Many things can cause blackheads to form, including increased oil production, hormones, and the presence of bacteria on the skin.
- To get rid of blackheads on the nose, experts recommend washing your face twice daily, using non-comedogenic skin care products, and avoiding squeezing blackheads.
Many of us have dealt with some form of acne at one point or another. After all, it is one of the most common skin conditions in the United States, affecting nearly 50 million Americans each year.1
In particular, blackheads also known as open comedones can be one of the most frustrating types of blemishes associated with acne because no matter how much scrubbing, cleansing, and exfoliating you may do, they don’t seem to go away.
According to Kellie Reed, MD, a board-certified dermatologist at Westlake Dermatology in Austin, Texas, blackheads can occur when pores on the face become clogged with oil, debris, or dead skin cells.
Genetics, hormonal factors, bacteria on the skin, and diet are other things that can cause blackheads to form as well, Reed told Verywell.
Blackheads can affect the face, neck, back, and chest, however, they most commonly occur on the nose due to the number of pores, hair follicles, and oil production in that area as well as the natural size of the pores, Anna Chien, MD, associate professor of dermatology and vice chair for Quality, Safety & Service at the Johns Hopkins School of Medicine, told Verywell in an email.
In some cases, blackheads can be deeply rooted into the pores, making it difficult to remove and often requiring the assistance of prescription grade products and/or a professional to extract them, Reed said.
Even though these pesky blemishes can be a pain to get rid of, there are some remedies you can try to treat them. Here’s how, according to dermatologists.
How to Get Rid of Blackheads on the Nose
Instead of picking or trying to squeeze your blackheads out, experts say there are home remedies, over-the-counter medications, and professional treatments that may help remove blackheads safely and naturally.
Home Remedies
- Green tea is a great antioxidant that can help reduce oil production in your skin.2 Mix green tea leaves with water and massage the leaves into your skin for about 30 seconds. Rinse off and apply a moisturizer afterward.
- Tea tree oil is another natural way to stop the growth of bacteria and can be found in many products, including soaps and creams.3 Apply tea tree oil directly to affected blackheads to prevent bacterial growth.
- Salt/sugar scrubs can help exfoliate the skin and remove dead skin cells on the skin’s surface. After massaging the scrub on your face, wash it off with water and apply a moisturizer.
- Baking soda just like salt and sugar scrubs can help exfoliate the skin and remove dirt, oil, and dead skin cells. Mix baking soda with water and massage it into any affected areas. Rinse off with warm water and use a moisturizer when done.
Over-The-Counter Treatments and Medications
- Azelaic acid can be found in topical creams and works by killing bacteria on your skin. This over-the-counter treatment can also reduce inflammation and keep the pores clean.
- Salicylic acid is an ingredient found in many cleansers, lotions, and creams. When it’s applied to the skin, it helps shed dead cells which can prevent pores and follicles from clogging.
- Benzoyl peroxide is another ingredient found in many over-the-counter products that work by lowering the amount of acne-causing bacteria on the skin.
- Topical retinoids can help prevent blackheads by decreasing oil production in oil glands and helping clear out clogged pores.
Professional Treatments
- Chemical peels contain certain acids like salicylic acid and beta hydroxy acid (BHA)s that help unclog pores and remove blackheads from the surface of the skin.
- Prescription-strength treatments are prescribed by a healthcare provider that works similarly to over-the-counter topical treatments like retinoids, however, they are stronger.
- Oral acne medications that are prescribed by a healthcare professional can help reduce bacteria that may cause blackheads.
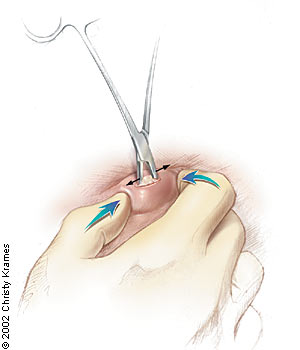
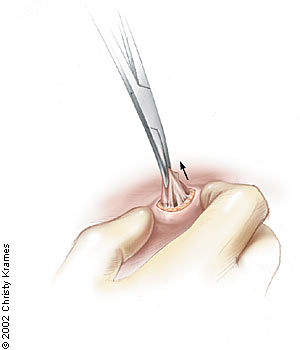
- Professional facials and removals or microdermabrasion treatments can remove dead cells and sebum that cause blackheads. A trained professional like an esthetician can extract blackheads safely during a facial treatment.
While certain methods and treatments like topical retinoids and other over-the-counter products can reduce oil production and help remove blackheads, using too much of any product can lead to dryness of the skin, redness, irritation, inflammation, or flakiness, Lindsey Bordone, MD, a board-certified dermatologist in the Department of Dermatology of Columbia University Medical Center, told Verywell in an email.
Methods and Treatments to Avoid
If you are trying to get rid of blackheads, especially on the nose, one of the biggest things you should avoid doing is squeezing them out of the skin or popping them, Chien said. While it can be tempting to squeeze them out yourself, you should leave it to the professionals to extract them, if needed.
“Excessive manipulation (squeezing, popping, etc,) should be avoided as it can lead to more inflammation and increase the risk for discoloration and scarring,” Chien added. “Excessive scrubbing and exfoliating should also be avoided.”
In addition, people should consider avoiding the use of pore strips because these products may cause more irritation than good, Reed said. “They often target surface debris and do little to resolve the deeper blackheads.”
How To Prevent Blackheads
Despite hormonal changes, genetics, and diet, Reed and Chien said there are some things you can do to prevent blackheads from forming. Here are some things that may help:
- Wash your face daily at least two times a day with a gentle or mild facial cleanser to remove oil, dirt, and other debris.
- Exfoliate two or three times a week to help remove dead skin cells from the surface of your skin.
- Use an oil-free moisturizer and sunscreen regularly to keep the skin hydrated without having to deal with excess oil production that can cause clogged pores.
- Swap out your products for non-comedogenic ones to avoid clogging the pores which can lead to the production of more blackheads.
- Remove makeup at the end of each day to avoid irritation from makeup products and to reduce the risk of clogged pores from oil, dirt, and dead skin buildup.
- Avoid touching or picking your face to prevent the spread of oil and bacteria from your hands.
- Rinse your face after any sweating to prevent dead skin cells and bacteria from getting into your pores.
When to See a Dermatologist
If you are following specific measures like washing your face daily and using certain over-the-counter medications, but they are not helping and you are not noticing any changes in your condition, it could be time to see a dermatologist for evaluation, Bordone said.
You should also schedule an appointment with a dermatologist if your condition is progressing and worsening, or if you are experiencing other symptoms such as increased inflammation, discoloration, or scarring of the skin, Chien said.
A professional can help manage your blackheads, provide other treatment options, such as prescription strength topicals, and in some cases, help remove them.
What This Means For You
Several methods and treatments can help get rid of blackheads. Experts recommend using over-the-counter treatments and medications like salicylic acid or benzoyl peroxide and maintaining a good and gentle skin care routine. If you don’t see an improvement or your blackheads worsen, it may be time to see a dermatologist.