Abscess Drainage: Procedures, Recovery, Recurrence
A skin abscess is a pocket of pus just under the surface of an inflamed section of skin. It’s usually triggered by a bacterial infection.
Abscess drainage is the treatment typically used to clear a skin abscess of pus and start the healing process. Smaller abscesses may not need to be drained to disappear.
Read on to learn more about this procedure, the recovery time, and the likelihood of recurrence.
Before a skin abscess drainage procedure, you may be started on a course of antibiotic therapy to help treat the infection and prevent associated infection from occurring elsewhere in the body.
The procedure is typically done on an outpatient basis. If you have a severe bacterial infection, you may need to be admitted to a hospital for additional treatment and observation.
Prior to making an incision, your doctor will clean and sterilize the affected area.
Usually, a local anesthetic is sufficient to keep you comfortable. It’s administered with a needle into the skin near the roof of the abscess where your doctor will make the incision for drainage. Examples of local anesthetics include lidocaine and bupivacaine.
The abscess drainage procedure itself is fairly simple:
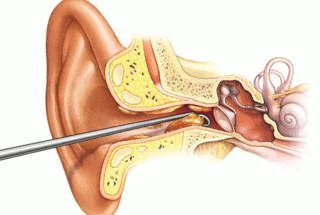
- Your doctor makes an incision through the numbed skin over the abscess.
- Pus is drained out of the abscess pocket.
- After the pus has drained out, your doctor cleans out the pocket with a sterile saline solution.
- The abscess is left open but covered with a wound dressing to absorb any more pus that is produced initially after the procedure.
- A deeper or larger abscess may require a gauze “wick” to be placed inside to help keep the abscess open. This allows the tissue to heal properly from inside out and helps absorb pus or blood during the healing process.
- Your doctor may send a sample of the pus to a lab for a culture to determine the cause of the bacterial infection.
Will you need a ride home?
If it isn’t possible to use local anesthetic or the drainage will be difficult, you may need to be placed under sedation, or even general anesthesia, and treated in an operating room. In this case, you’ll need a ride home.
If a local anesthetic is enough, you may be able to drive yourself home after the procedure. If the abscess is in a location that may affect your driving, such as your right leg, you may need a ride.
Recovery time from abscess drainage depends on the location of the infection and its severity.
The gauze dressing on the skin over the wound incision may need to be in place for a couple of days or a week for an abscess that was especially large or deep.
If this dressing becomes soaked with drainage, it will need to be changed.
If your doctor placed gauze wick packing inside of the abscess cavity, your doctor will need to remove or repack this within a few days.
You can expect a little pus drainage for a day or two after the procedure.
Your doctor may also prescribe antibiotic therapy to help your body fight off the initial infection and prevent subsequent infections. Pain relieving medications may also be recommended for a few days.
Within a week, your doctor will remove the dressing and any inside packing to examine the wound during a follow-up appointment. If everything looks good, you may be shown how to care for the wound and change the dressing and inside packing going forward.
For the first few days after the procedure, you may want to apply a warm, dry compress (or heating pad set to “low”) over the wound three or four times per day. This can help speed up the healing process.
You may also be advised to gently clean the area with soap and warm water before putting on new dressing. However, you should check with your doctor or a nurse about home care.
Healing could take a week or two, depending on the size of the abscess. During this time, new skin will grow from the bottom of the abscess and from around the sides of the wound.
An abscess doesn’t always require medical treatment. Milder abscesses may drain on their own or with a variety of home remedies.
You may be able to help a small abscess start to drain by applying a hot, moist compress to the affected area. This may also help reduce swelling and start the healing.
Other treatments for mild abscesses include dabbing them with a diluted mixture of tea tree oil and coconut or olive oil.
Soaking a cloth compress in hot water and Epsom salt and applying it gently to an abscess a few times a day may also help dry it out.
A skin abscess, sometimes referred to as a boil, can form just about anywhere on the body. A blocked oil gland, a wound, an insect bite, or a pimple can develop into an abscess.
If the infected area of your current abscess is treated thoroughly, typically there’s no reason a new abscess will form there again.
However, if the infection wasn’t eliminated, the abscess could reform in the same spot or elsewhere. Taking all of your antibiotics exactly as prescribed can help reduce the odds of an infection lingering and continuing to cause symptoms.
An abscess can also form after treatment if you develop a methicillin-resistant Staphylococcus aureus (MRSA) infection or other bacterial infection. These infections are contagious and can be acquired in a hospital setting or through direct contact with another person who has the infection.
Your doctor will treat an MRSA abscess the same as another similar abscess — by draining it and prescribing an appropriate antibiotic.
The most obvious symptom of an abscess is a painful, compressible area of skin that may look like a large pimple or even an open sore. The skin around the abscess may look red and feel tender and warm. You may also see pus draining from the site.
Other symptoms may include:
- swelling around the infected area
- hardened outer layer of skin
- fever or chills if the infection is severe
A small abscess with little pain, swelling, or other symptoms can be watched for a few days and treated with a warm compress to see if it recedes. You should see a doctor if the following symptoms develop:
- The abscess grows.
- You see pus (which is usually a sign of infection).
- Redness and swelling forms around the sore area.
- The area is warm to the touch.
- You have a fever or chills.
A doctor can usually diagnose a skin abscess by examining it. You should also be able to answer questions about your symptoms, such as:
- when the abscess formed
- whether it’s painful
- whether you’ve had other abscesses
To identify the type of infection you have, your doctor may send pus drained from the area to a lab for analysis.
Abscess drainage is usually a safe and effective way of treating a bacterial infection of the skin. A doctor will numb the area around the abscess, make a small incision, and allow the pus inside to drain. This, and sometimes a course of antibiotics, is really all that’s involved.
If you follow your doctor’s advice about at-home treatment, the abscess should heal with little scarring and a lower chance of recurrence.